Suite 3, Ground Floor, The Gateway,
312 St Kilda Road, Southbank, VIC, 3006
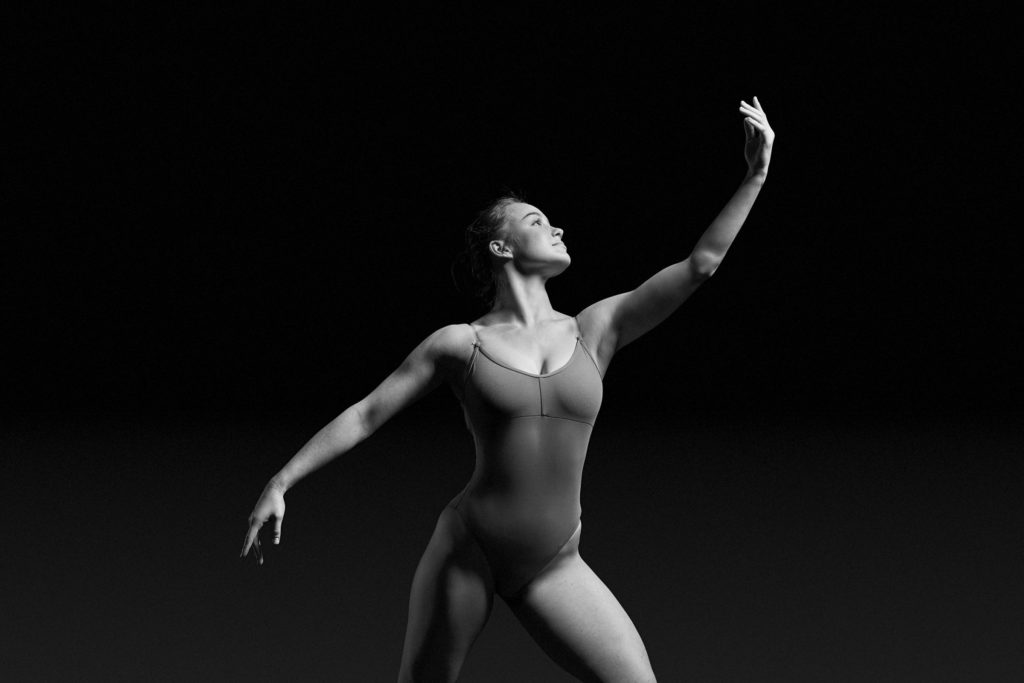
Dance Injuries
At Performance medicine we are experts in dance physiotherapy at are at the forefront of the performing arts industry. You’re in the right place to manage any dance related concerns.
We are a collective of experts and experienced physiotherapists and performance medical practitioners. Our team create a uniquely accepting space for all performers of all abilities to rejuvenate and re-energise their greatness.
We treat dance injuries as we do all things, with customised tailored recovery programs that provide you with a safe and supportive environment to recover. Get your recovery under way and come see us today.
Some common dance injuries include:
- Anterior Hip Impingement
- Hip labrum tears
- Posterior ankle impingement
- FHL tenosynovitis
- 2nd Metatarsal stress fracture
- High Hamstring Strain
- REDS-s (Relative Energy Deficiency in Sport – Syndrome)
Anterior Hip Impingement
Anterior hip impingement is pain or discomfort at the front of the hip. It is commonly in response to muscle imbalances around the hip and the subsequent irritation of the synovial tissues of the hip joint capsule.
Dancers have a higher risk of developing this condition, as they are required to use large ranges of hip movement and have high loads of training.
Signs and symptoms of anterior hip impingement may include, a pinching sensation at the front of the hip and sometimes clicking may be present prior to the hip hurting.
Physiotherapy management involves decreasing hip pain to restore hip range via soft tissue and joint techniques. This is followed by specific strengthening of the deep hip rotators, lower glutes, adductor muscles and improving lumbopelvic control.
Hip Labrum tears
The labrum of the hip is a suction cup that helps you maintain good hip joint biomechanics. Research has shown that labral tears of the hip may be common in dancers, however, a labral tear may not be the source of your hip pain. There are many other structures of the joint that may contribute to your hip pain including the joint capsule and muscle imbalance. It is important to seek a dance specific physio assessment and rehabilitation program to strengthen the deep hip muscles to support your hip whether you seek surgical advice or not.
Why hip surgery isn’t a silver bullet
Posterior ankle impingement
You may have posterior ankle impingement if you are experiencing pain, discomfort or puffiness at the back and sides of your ankle. You might experience this when you point, plie, rise or jump and this pain may be increasing.
Posterior ankle impingement is generally caused by irritation of the structures in your ankles (fat pads and bursae). In some cases, it may be associated with FHL (flexor Hallucis Longus) tenosynovitis. You may find that rest does help but it returns again when you start to rise or releve.
Ice is useful in reducing pain, swelling and irritation behind the ankle but the primary treatment includes biomechanical retraining and strengthening of your ankle and foot.
FHL (Flexor Hallucis Longus) Tenosynovitis
The FHL is a muscle of the lower leg and foot whose primary function is to pointe the big toe and the it also contributes to pointing your ankle. The FHL’s journey from the leg to the toe involves it travelling along the inside part of your ankle past bony groove or tunnel. To assist the tendon glide and slide nicely when you pointe and plie, it is surrounded in a sheath. This sheath may become inflammed behind the inner part of the ankle particularly in ballet dancers. FHL is susceptible to high loads with jumping, pointing and dancing en pointe. When overload occurs in this muscle, the tendon rubs excessively in the bony groove. This causes an inflammatory response in the tendon sheath (i.e. tenosynovitis).
If you are experiencing FHL tenosynovitis, you may experience pain anywhere along the FHL tendon, weakness in pointing/jumping/pointe work; a reduced range of pointe and pinching at the back of the ankle.
2nd Metatarsal Stress Fracture
A stress fracture of the second metatarsal is more common in ballet dancers due to the high load and overuse of releve, rises and en pointe work. Signs and symptoms of a stress fracture often include localised and pain over the middle of the foot with pain increasing with with walking and en pointe.
Stress fractures are often difficult to see via plain X-ray therefore diagnosis may be through clinical assessment by your physiotherapist or doctor, an MRI or bone scan.
Retraining your foot biomechanics and strength work with your physiotherapist are primary parts of your rehabilitation as your bones recover and become strong again.
Relative Energy Deficiency in Sport (RED-S)
The syndrome of RED-S refers to the impaired physiological functioning of dancer or athlete caused by relative energy deficiency. This includes, but is not limited to, impairments of metabolic rate, menstrual function, bone health, immunity, protein synthesis and cardiovascular health. As well as this, RED-S affects a dancer’s performance by decreasing endurance, muscle strength, coordination and concentration and increasing the risk of injury and depression. There is a disproportionate high prevalence of RED-S in the dance community but very little awareness or education into the area. At Performance Medicine, we are working together with international experts to create treatment programs that allow you to have a happy and sustainable dance career.
Hamstring Strain
Hamstring tears often occur when the muscles are eccentrically contracting (contracting whilst lengthening) and at high speed, for example when you are doing a high leg kick. In the dance population, hamstring tears may also occur in slow stretching. This can be from practising the splits or holding the splits for long periods of time and is most common when your muscles are fatigued.
If you sustain a hamstring tear you may experience pain, tenderness and weakness in the back of your thigh (which may radiate up to your buttock).
Treatment and management of your hamstring strain should include a detailed physiotherapy assessment. It’s important to determine the severity of the strain and the appropriate strength and retraining your muscle or technique all whilst keeping you in the studio.

Related Treatments
Related Practitioners
Dr Suleiman Halabi (he/him)
Sports Doctor - M.B.B.S.
Rhea Torres (she/her)
Physiotherapist - DPT. BNSc. BSc.
Annie Strauch (she/her)
Managing Director - Titled Physiotherapist - MACP
Nino La Scala
Titled Physiotherapist
Elise McMahon (she/her)
Physiotherapist
Letitia Reus (she/her)
Physiotherapist - APAM
Elissa Petesic (she/her)
Physiotherapist - APAM
Emily McLean (she/her)
Physiotherapist - B.Physio Adv. (Hons), Masters of Sport Physio
Stephanie Zamoyski (she/her)
Senior Physiotherapist - B..HthSci & M.Phty
Maria Anagnostou (she/her)
Clinical Director Sydney - Titled Physiotherapist, MACP
Zeba Haroon (she/her)
Physiotherapist
Chris Minto (she/her)
Senior Physiotherapist
Polly Dhar (she/her)
Senior Physiotherapist - APAM
Nicole Reynolds (she/her)
Senior Physiotherapist - APAM
Dr Kathy Yu (she/her)
Sports Doctor - M.B.B.S.
Stacey Kipouridis (she/her)
Physiotherapist - APAM
Catherine Etty-Leal (she/her)
Clinical Director Melbourne - Titled Physiotherapist, MACP