Suite 3, Ground Floor, The Gateway,
312 St Kilda Road, Southbank, VIC, 3006
The “TMJ” – What is it and why does it hurt?
During their lifetime about two thirds of the population will experience “TMJ pain” or “TMD”. Many of the population will live for years with “TMJ problems” before having their problem accurately diagnosed and effectively treated. But what exactly is the “TMJ” and why is it so problematic?
Terminology
“TMJ” stands for temporomandibular joint, commonly known as the jaw joint. Everyone has two TMJs, one on either side of the face and it is important that these joints work simultaneously in a co-ordinated fashion to maintain happy, healthy joints. The term “TMJ” often gets confused with “TMD”, which stands for temporomandibular dysfunction. TMD is an umbrella term describing pain or dysfunction in the jaw joints.
Anatomy
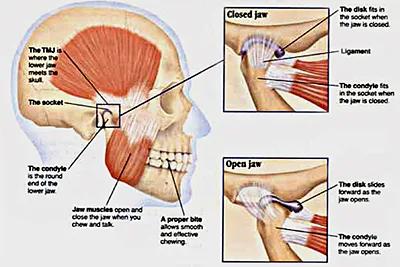
The TMJ is essentially a ball and socket joint. Like other joints in the body, it is surrounded by a fibrous joint capsule and contains synovial fluid that acts as a lubricant for the joint. It is one of the more unique joints in the body as it has a disc that runs between the two joint surfaces, dividing the joint into two compartments, each acting somewhat like an independent joint. The disc attaches to the capsule so that it can glide easily within the joint as we open and close our mouth. The disc has highly vascular tissue connecting it to the mandible and this tissue can be a source of pain when there is inflammation or compression in the TMJ.
When Things Become Problematic…
Jaw pain often increases over time and can be precipitated by an event such as biting into something hard with increased effort, wisdom teeth removal, orthodontic work or a long session at the dentist. Pain is often felt over the jaw and can refer into the ear, teeth, back of the neck or head. Clicking may also be a symptom of TMD and this may or may not be painful. In any case, TMJ clicking should not be ignored as it can progress into more serious issues with the jaw including inflammation and pain.
What can I do if I have TMJ Pain?
If you have any clicking, pain or stiffness, the Performance Medicine Physiotherapists can certainly help you decipher what is going on with your jaw. Physiotherapy is one of the most effective ways to manage jaw problems, however in some situations a specialised splint may be required to protect your teeth from erosion secondary to grinding (fitted by your dentist). Very rarely is surgery required to manage jaw pain and dysfunction.
You do not need a referral to see a physiotherapist for jaw problems. Your physiotherapist will thoroughly assess your jaw and determine which structure is the primary cause of your problems. You will then be treated with a variety of soft tissue and joint techniques, as well as being given exercises to mobilise and/or strengthen your jaw. Your physiotherapist will also play an important part in educating you how to retrain the normal biomechanics of your jaw in order to prevent your jaw problems returning.
So to stop that pain when you bite into your favourite food, please call Performance Medicine on 9820 1324 or email info@performancemed.com.au
Catherine Worsnop B. Phty, APAM Physiotherapist Certified APPI Pilates Matwork Instructor
Picture sourced and acknowledged from: http://morphopedics.wikidot.com/tmj-syndrome