Suite 3, Ground Floor, The Gateway,
312 St Kilda Road, Southbank, VIC, 3006
Proximal Hamstring Tendinopathy: A Real Pain in the Butt
What is Proximal Hamstring Tendinopathy ?
Proximal hamstring tendinopathy (PHT) is a condition that results in a painful tendon in the lower buttock area1,2. Pain may also radiate down the back of the thigh2.
PHT is an overuse injury that most commonly affects runners, dancers, and other change of direction sports (e.g. hockey and football). It can also occur in Pilates, yoga and non-sporting populations2.
PHT can be a frustrating condition to manage, and symptoms may persist for an extended period, ranging from months to even years2. For this reason, it is important that we make an accurate diagnosis and provide a comprehensive rehabilitation plan1,2.

Where can the pain be felt?

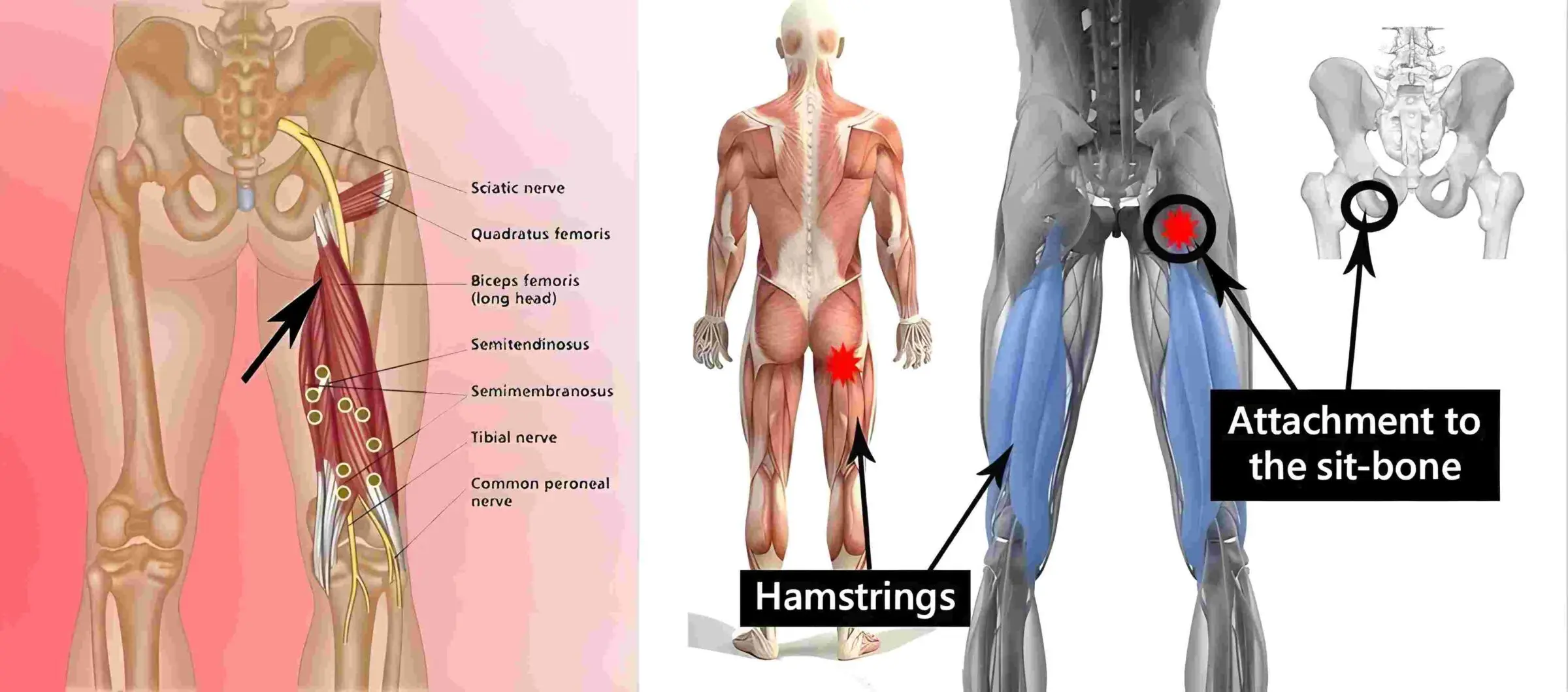
We have three hamstring muscles at the back of our thigh. They connect to the pelvis through the hamstring tendon onto a common attachment point on the ischial tuberosity (sit bones). The area where our sit bones are is where the pain can be felt, especially when sitting.
How does PHT occur?
Tendons connect muscles to bones and don’t like being asked to do too much, stretched or compressed1. When the hip is moved into flexion (knee toward your chest), the hamstring tendon wraps around its attachment on the sit bone and creates a compressive force. Two examples of activities that include this movement are sitting in a low chair, or high kicks in dancing.
What does it feel like?
- Deep pain, tenderness or stiffness in the buttock (around sit bone)1
- Pain with sitting or pressure on the area1
- Pain with bending forward (e.g. putting on your shoes, packing the dishwasher, gardening, picking up items off the ground)2
- Pain with deep hip flexion (knee to chest): squatting, lunging, sprinting, walking upstairs, running up hills, sitting in a low chair (e.g. driving in the car)2,3

How do we treat PHT?
The key to managing tendinopathy is a progressive loading program, using pain to guide how fast we can progress through the rehabilitation2. Injection therapies are commonly suggested, however there is only very low evidence available for their use.4
Stage 1 (reduce pain and gentle strengthening):
- Reducing compression is key to help the tendon settle1,2
- Anti-inflammatories may be recommended1,2
- Adjustments in training to avoid unnecessary load and compression is very important2
- Isometric exercises (e.g push and hold resistance without moving) are used to settle tendon pain and introduce a gentle amount of loading for the tendon2
Stage 2 (strength work in positions of no compression):
- A variety of strength exercises are used to address various aspect of hamstring strength1
- Compression is avoided (minimal or no hip flexion)2
- Training loads are still monitored closely, ensuring the re-introduction of any aggravating activities (e.g. sitting, high kicks, running etc) is slow/gradual and doesn’t provoke symptoms.
Stage 3 (strength work and gradually adding compression):
- Harder strength exercises are introduced in this stage
- Introduction of greater hip flexion (knee to chest) are slowly introduced, being guided by symptoms.1,2
Stage 4 (power and explosive exercises):
- Fast and explosive exercises that put extreme loads through the hamstring to ensure it’s ready for return to sport1,2.
- This stage is reserved only for people who are aiming to return to highly explosive sports that require lots of running, jumping, landing etc.

How long does rehab take?
Rehabilitation for proximal hamstring tendinopathy may take between 3-6 months, or even longer. It is variable between people, and there are many factors influencing how long the rehabilitation can take2.
It is important to remember that all tendons in the body are slow to improve. For this reason, ensuring you complete the entire rehabilitation journey will help to get your hamstring back to full function.
Conclusion:
Proximal hamstring tendinopathy can be a challenging and persistent condition, but with the right diagnosis and a structured rehabilitation program, recovery is achievable. By gradually strengthening the hamstring while managing compression and load, we can help reduce pain and restore function. If you’re experiencing symptoms, seeking professional physiotherapy guidance from the team at Performance Medicine will ensure you receive a tailored plan for a safe and effective recovery. Book in with us today!
References:
1. Beatty NR, Félix I, Hettler J, Moley PJ, Wyss JF. Rehabilitation and Prevention of Proximal Hamstring Tendinopathy. Current Sports Medicine Reports. 2017;16(3):162–71.
2. Goom TSH, Malliaras P, Reiman MP, Purdam CR. Proximal Hamstring Tendinopathy: Clinical Aspects of Assessment and Management. The journal of orthopaedic and sports physical therapy. 2016;46(6):483-493. doi:10.2519/jospt.2016.59863.
3. Lempainen L, Johansson K, Banke IJ, et al. Expert opinion: diagnosis and treatment of proximal hamstring tendinopathy. Muscles, Ligaments and Tendons Journal. 2019;5(1):23. doi:10.32098/mltj.01.2015.05
4. Nasser AM, Vicenzino B, Grimaldi A, Anderson J, Semciw AI. Proximal Hamstring Tendinopathy: A Systematic Review of Interventions. International journal of sportsphysical therapy. 2021;16(2):288-305. doi:10.26603/001c.21250
5. Image 1: Available from: https://sinicropispine.com/wp-content/uploads/2015/04/34943053_l.jpg
6. Image 2: Available from: https://www.patcarton.ie/3d-images/hamstring-tendon-repair.jpg
7. Image 3: Available from: https://www.sportsinjurybulletin.com/AcuCustom/Sitename/DAM/094/10881-ham-fig-1.jpg
8. Image 4: Goom TSH, Malliaras P, Reiman MP, Purdam CR. Proximal Hamstring Tendinopathy: Clinical Aspects of Assessment and Management. The journal of orthopaedic and sports physical therapy. 2016;46(6):483-493. doi:10.2519/jospt.2016.59863.